The Medicare Advantage Special Needs Plans (SNPs) landscape is evolving, driven by new CMS regulations aimed at improving care for individuals with complex health needs – including those eligible for both Medicare and Medicaid. These changes are redefining how SNPs deliver services, with a focus on better coordination, expanded benefits, and simplified enrollment. This post outlines the most significant 2025 updates, including plan growth, mandatory benefit enhancements, and tighter integration between Medicare and Medicaid, and explores what they mean for your organization and its stakeholders.
In 2025, the total number of available SNP plans increased, and has more than doubled since 2018:
- 1,445 SNPs are available across the country, an uptick of 8% over 2024
- The total number of C-SNP plans reached 376 and total enrollment has grown by 67%1
- Since 2018, the number of D-SNPs has grown from 401 plans to 909 plans today. Nearly two-thirds of SNP plans are dedicated to beneficiaries with both Medicare and Medicaid.1
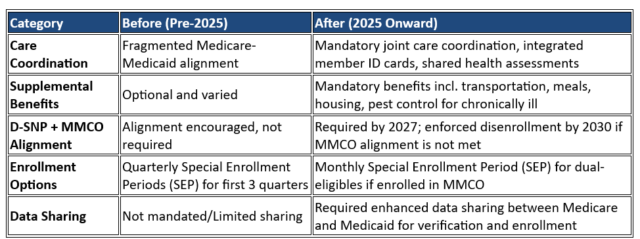
CMS has introduced new regulations for 2025 that strengthen and standardize offerings such as transportation, meals, and care coordination which have been made mandatory. Care coordination must be jointly managed by Medicare and Medicaid, including the use of integrated member ID cards and joint health assessments, with implementation expanding progressively from 2025 through 2027.
Beginning in 2027, Dual Eligible Special Needs Plans (D-SNPs) will be required to coordinate with affiliated Medicaid Managed Care Organizations (MMCOs). To stay enrolled in a D-SNP, beneficiaries will also need to be enrolled in the corresponding MMCO. By 2030, individuals who are not aligned with the affiliated MMCO will be disenrolled from the D-SNP.2 Plans must ensure that beneficiaries are enrolled in both the D-SNP and the affiliated MMCO, which requires enhanced data sharing and verification processes between Medicare and Medicaid systems.
In January 2025, CMS implemented a new monthly Special Enrollment Period (SEP) for dual-eligible beneficiaries. This SEP allows individuals to enroll in D-SNPs monthly, provided they are also enrolled in the affiliated MMCO. These changes are designed to improve care coordination, simplify enrollment and ensure that enrollees receive more integrated, comprehensive support across both Medicare and Medicaid. Administrators must adjust systems to manage new monthly SEPs which means tighter coordination to process enrollments and disenrollments more frequently and accurately.
More Medicare Advantage plans, especially SNPs, are offering supplemental benefits for the chronically ill to address social determinants of health, including meals with an increase in produce, housing supports, transportation for non-medical needs, and pest control.2 These benefits are particularly prevalent in D-SNPs, with 93% offering meals, compared to 15% in general Medicare Advantage plans.3 Admin teams must develop new vendor relationships, track benefit usage, and educate beneficiaries about these benefits. Increased regulatory scrutiny means administrators must accurately document these expanded benefits and report on their effectiveness.
Medicare SNP Changes – Before vs. After (2025 and Beyond)
Overall, the program changes will have a positive impact on SNPs, with total enrollment projected to exceed 7 million in the coming year. These advancements will support beneficiaries eligible for both Medicare and Medicaid in transitioning to fully integrated or highly integrated plans, improving health outcomes while also helping to manage costs more effectively.
SNP plan administration in 2025 is more complex, requiring enhanced coordination across Medicare and Medicaid, expanded benefit management, improved data reporting, and stronger compliance efforts. RAM Technologies plays an important role in enabling the successful deployment and administration of Special Needs Plans through a fully integrated solution that combines advanced technology, operational expertise, and regulatory compliance alignment.
Key benefits include but are not limited to:
- End-to-End Technology and Services Platform: HEALTHsuite Advantage, integrated portals for members and providers, and BPaaS streamline all core administrative functions
- Comprehensive Operational Services: Includes enrollment, billing, claims, call center, compliance, and more
- Regulatory Alignment: Built-in CMS integration, reporting, and audit support ensure ongoing compliance
- Scalable, Secure Infrastructure: Hosted in a state-of-the-art facility with 24/7 support and disaster recovery
- Rapid Implementation: Our preconfigured implementation approach reduces deployment time and complexity
Reach out to us today to learn more about how RAM leverages SaaS and BPaaS deployment models to help reduce risk, minimize staffing burdens, and focus on delivering high-quality care to members.
References
1Meredith Freed, Jeannie Fuglesten Biniek, Anthony Damico, and Tricia Neuman, Medicare Advantage 2025 Spotlight: A First Look at Plan Offerings (Kaiser Family Foundation, 15 November 2024)
2Contract Year 2025 Medicare Advantage and Part D Final Rule (CMS-4205-F)
3Claire B. Cruse Joseph June Tyler Cromer Davis Baird Kali Peterson Narda Ipakchi, Centering Beneficiaries’ Perspectives Amidst Change In The Medicare Advantage Supplemental Benefits Environment Rule (Health Affairs, 6 December 2024)

